Weekly volume and dosimetric changes during chemoradiotherapy with intensity-modulated radiation therapy for head and neck cancer: a prospective observational study. (http://www.ncbi.nlm.nih.gov/pubmed/20338474)
Bhide SA, Davies M, Burke K, McNair HA, Hansen V, Barbachano Y, El-Hariry IA, Newbold K, Harrington KJ, Nutting CM.
Int J Radiat Oncol Biol Phys. 2010 Apr;76(5):1360-8.
Saturday, April 17, 2010
Things aren't always what they seem at first
Sunday, April 11, 2010
The Master speaks
So, it's good that he issues refreshers like this one to keep our management strategies abreast with latest developments.
This appears as the article 'Current management strategy of nasopharyngeal carcinoma' in Clin Exp Otorhinolaryngol. 2010 Mar;3(1):1-12
(http://www.ncbi.nlm.nih.gov/pubmed/20379395)
Other review articles of relevance are linked as well.
(http://www.ncbi.nlm.nih.gov/sites/entrez?db=pubmed&cmd=link&linkname=pubmed_pubmed&uid=20379395)
New in OSA
Authors Xu H, Huang W, Yu L, and Chen L. published in Acta Otolaryngolica this week an article entitled 'Sound spectral analysis of snoring sound and site of obstruction in obstructive sleep apnea syndrome.'
(http://www.ncbi.nlm.nih.gov/pubmed/20377505)
They showed objectively what we have known intuitively, that the higher the obstruction the lower the pitch of noise generated. In fact they found that lower obstructions had a greater proportion of >800Hz and >2000Hz first-snore sounds than higher obstructions.
This confirms the way we clinically differentiate stertor and stridor, and might even spawn a new wave of polysomnogram parameters.
Thursday, November 12, 2009
I can tell by the way you snore...

Wouldn't it be great if we didn't have to do expensive polysomnograms, read incomprehensible charts, and (in the public setting) wait for months for a sleep study? All just to diagnose OSA and say to a patient ok, now we are sure you need treatment. Especially when he's been falling asleep in your waiting room or just come in with head bandaged after his lorry overturned. You know he has OSA.
Well, it seems the people in Brisbane have found a way.
I have been thinking along the lines of a biochemical marker or something that might be detected in the breath. Imagine bus drivers having to check in for a urine test or breathalyser test before they board and you get the idea.
The sleep team in University of Queensland have reported they can HEAR that you have OSA.
I guess I have always had this hunch. Haven't you? There's a rhythmic hiss in the meeting room and you thought it was the air-condition vent until the guy next to you starts nodding. You think the ventilator is leaking when you realise your assistant in OR is stertoring. You know. Nothing scientific. No data to base this on. Just that visceral hunch that there's no way you can be breathing right during sleep if you are hissing with every breath through the day.
But these guys down under have made a science of it and claim over 90% sensitivity and specificity by simply analysing the audio recording of your snore!
Read the Article at HealthJockey.com
Review the scientific papers related to snoring by their lead researcher Dr. Udantha Abeyratne.
Tuesday, November 10, 2009
Post exposure prophylaxis for Varicella?

The author of this blog is currently in day 7 of illness, suffering from a moderate form of varicella. In spite of starting acyclovir (thanks to vigilant and quick-acting wife) on the day of eruptions, the disease process was not halted and vesicles are florid. While we are taking precautions against pneumonia, encephalitis, and other adult-onset associated complications, it is my 2yr old that I agonise about.
He is an 'exposed' individual. Varicella infections in children are mild and rarely complicated. Being an otolaryngologist, however, we know that Ramsay-Hunt (herpes zoster oticus; i.e. reactivation of virus in facial nerve) syndrome causes debilitating facial palsy - sometimes irreversible. Shingles is painful, too. My question is, should I bother vaccinating him now? He was planned for his jab next week, but now that he is exposed, shouldn't I just wait and see if he develops the infection which would obviate vaccination altogether?
Well, this is where the evidence is really useful:
According to the Cochrane review of randomized trials evaluating varicella vaccine in children and adults; from 3 trials with 110 healthy siblings of household contacts where they received post-exposure prophylaxis (PEP) within 3 days of exposure or not at all:
- varicella developed in 18% (PEP) vs. 78% (no PEP) (p < 0.05)
- moderate to severe varicella developed in 2% (PEP) vs. 76% (no PEP) (p < 0.05)
- PEP group who developed varicella had mild disease (< 50 skin lesions)
- no trials reported on adverse events following immunization
Also, for all my healthcare worker friends out there, don't be a hero (or a chicken, depending why you're delaying.) Get yourself jabbed now! Varicella vaccine is recommended for those who have never had chickenpox and are seronegative for varicella antibodies. The caveat (or bonus) is 1-5% adult develop varicella-like rashes that shed the virus and should be removed from patient contact (perfect excuse for holiday, no?) [Am Fam Physician 1997 Dec;56(9):2291]
Tuesday, October 27, 2009
Unilateral hearing loss: To MR or not to MR?
Perhaps our suspicion index can be guided by the symptom profile of acoustic neuroma where there is:
93.4% hearing impairment
75.5% tinnitus
40.6% vertigo
38.8% unsteadiness
Hearing loss can be sudden (12-47%) or insidious
Ho & Kveton, 2002, recommended a protocol for investigation:
- for patients with limited symptoms (isolated vertigo, historically explained unilateral hearing loss or tinnitus, or symmetrical hearing loss; estimated risk of acoustic neuroma < 5%): ABR as initial test and MRI if abnormal ABR
- for patients with intermediate symptoms (sudden sensorineural hearing loss or unexplained persistent unilateral tinnitus; estimated risk of acoustic neuroma 5-30%): MRI as initial test
- for high-risk patients with combination of unilateral asymmetric sensorineural hearing loss, tinnitus and decreased speech discrimination (estimated risk of acoustic neuroma > 30%): MRI with gadolinium initially and periodic ABR testing if negative MRI
On the other hand, it is worth remembering that tumor growth is on average 1-2.3 mm/year and less than 30% grow > 2 mm/year so that serial MRIs are hardly helpful and may not require any intervention in the elderly.
References
Arch Otolaryngol Head Neck Surg 2004 Feb;130(2):216
Neurosurgery 2006 Jul;59(1):67
J Laryngol Otol 1994 Feb;108(2):116
Am J Otolaryngol 1999 May-Jun;20(3):157
Neurosurgery 1997 Jan;40(1):1
Otolaryngol Clin North Am. 2002 Apr;35(2):393-404, viii
Friday, January 16, 2009
Risk of CA in MNG

I was asked this by a friend who has a progressively enlarging non-toxic goitre and a CT scan that showed a huge multinodular goitre with tracheal compression: do I need surgery and why? Should the whole thyroid be removed or can some be spared?
My quick answer was YES you need surgery, and a total thyroidectomy, both because of the risk of occult carcinoma. An FNAC can easily miss malignant foci, MNGs have a risk of malignant change, imaging has no reliable sign of malignancy, and compression heralds worse complications (with or without op).
But what's the risk exactly, and what does evidence say about how much of thyroid to remove? This is what the evidence says:
1)In a review of 317 patients operated for multinodular goiter, the incidence of occult micro-carcinoma was 3.3% (Wahl RA, Goretzki P, Meybier H, Nitschke J, Linder M, Roher HD. Coexistence of hyperthyroidism and thyroid cancer. World J Surg 1982; 6: 385-390)
2) Another review of 98 total thyroidectomies done for MNGs revealed an incidence of 10 cases (10.2 percent) occult carcinomas - seven patients were diagnosed with papillary carcinoma, two with the follicular variant of papillary and one with follicular carcinoma.
http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijs/vol17n1/goiter.xml
2) Total thryoidectomy may avoid need for reoperation in case of incidental thyroid
cancer; a study of 218 patients with euthyroid multinodular goiter and no suspicion for malignancy were randomized to total or near-total thyroidectomy (remnant tissue < 1 g) vs. bilateral subtotal thyroidectomy (remnant tissue> 5g); no significant differences in rates of temporary unilateral vocal cord dysfunction (0.9% vs. 0.9%), hypoparathyroidism (1.8% vs.0.9%) or finding of papillary cancer (9.2% vs. 7.3%) (Arch Surg 2004 Feb;139(2):179 in JAMA 2004 May 5;291(17):2058)
So, with a risk of somewhere between 3-10% occult carcinoma (papillary still being the commonest) and near-total also mean could-miss; I think it's still right to say MNGs should be treated with total thyroidectomies unless surgically difficult; upon which post-operative suppressive thyroxine may be an option.
Saturday, April 19, 2008
Proud flesh
One rarely sees proud flesh outside of the diabetic foot these days, what more in the neck. This patient had a badly infected tracheostomy and was taken of it for a couple of weeks for Pseudomonas infestation. This is the result of a wound desperately trying to fill the gaps with granulation tissue while never being able to epithelialise.
What I had to do was to excise the entire granulating mass with a cuff of skin, all the way down to the strap muscles before redoing the tracheostomy. Wound care is going to be very important for this not to happen again.
Monday, April 07, 2008
Microflap excision

These vocal cords belong to a middle-aged chronic smoker who has suffered from a hoarse voice for close to a year. His wife has been my patient for many years and she decided to bring him to see me. As you can see there is intense leukoplakia on both vocal cords. A CT scan revealed no framework infiltration or extension into the pre-epiglottic space. I had tried several biopsies using a flexible scope but tissue was inadequate.

I put him under for a proper microflap excision today. Seen here is the epithelium and subepithelial layers raised, revealing the vocal ligament and gelatinous lamina propria covering it. One advantage of doing this is that I can directly inspect for deep infiltration and also examine the ventricle and subglottic space (which were free growth).

As the free edge of the vocal cord was not spared by this exophytic lesion, it didn't seem logical to confine my excision to the dorsal surface only. After all, voice-sparing was no longer my concern. More important was to get a good representative specimen. The dilemma/temptation was to get some tissue from the opposite vocal cord but thankfully caution prevailed. Last thing I need is an adhesion anteriorly and ruin his voice forever.
Should the lesion be non-invasive, I can still go in again to do the other side. If it's malignant then some radical modality will be offered. That's the plan.
Wednesday, April 25, 2007
GERD in the News
The study shows the RDQ to be a valid and reliable questionnaire with excellent construct validity and a good relationship to quality of life. The diagnostic value of the RDQ in primary care is limited, but combination with an additional proton pump inhibitor treatment course might improve the RDQ's ability to discriminate GORD patients according to their symptom association probability outcome.
Medical News Today
Heartburn could be a precursor to gastro-oesophageal reflux disease, British doctors warn and note that the diagnosis of the disease is a relatively new phenomenon. Statistics show that over a quarter of Britons have gastro-oesophageal reflux disease, also known as the GORD, and thousands of these are not getting the treatment they need. A noted general practitioner, Dr Rob Hicks, said that the GORD as a diagnosis was a relatively new phenomenon and that although most medical practitioners were aware of it, many patients could still be suffering in ignorance. "What we are trying to do is to raise awareness, because there are many people still suffering from heartburn two or three times a week. I would advise them to see their doctor," Hicks said.
MedIndia.com
Powered by ScribeFire.
Monday, April 17, 2006
Combined Approach to Paranasal Sinuses
This article first reviews the historical development of FESS, from Wigand's postero-anterior approach (expose posterior ethmoids, open face of spehnoid, and retrograde ethmoidectomy) to the antero-posterior approach of Messerklinger & Stammberger (anterior ethmoidectomy followed by antegrade dissection posteriorly, extent determined by disease.) Kennedy's FESS is built on these antecedent techniques with the aim of 'reestablishing sinus drainage & mucosal recovery through restoration of obstructing sinus ostium and removal of devitalised mucous membrane or bone.'
The obvious advantage and disadvantage of the P-A approach is that
1. it avoids the skull base
2. surgery is excessive in cases of limited disease
As for the A-P approach:
1. surgery is selective and limited to pathologic sinus
2. there is potential for penetrating the posterio-inferiorly sloping skull base
The author's (Schaeffer) CAPS (combined approach to paranasal sinuses) is introduced and discussed. It is claimed that CAPS aims to 'bring together the salient features of the AP and PA approaches while observing the concept of functional endoscopic sinus surgery' and is therefore a 'minimally invasive surgery.. seeking the least disruption of form and function of the paranasal sinuses'
Key tenets of the combined approach are :
1. It is a 'disease-and-anatomy-oriented surgical approach'
2. It's goal is to 'conserve sinus anatomy'
3. Surgical principles utilizes 'anatomic relationships'
(It is disease-oriented in that surgery is targeted to 'relieve medically irreversibly obstruction of sinus outflow tracts' and it is anatomy-oriented in that anterior and posterior ethmoid sinuses are approached separately, in view that they are 'embryologically distinct structures... separated by the basal lamella of the middle turbinate.')
The key surgical principles include:
1. Complete uncinectomy necessary for anterior ethmoidectomy and prevent recurrence
2. Identification of MSO necessary to find plane of lamina papyracea
3. Anterograde (AP) dissection of anterior ethmoid cells up to basal lamella, retrograde (PA) dissection of posterior ethmoid cells
The authors' experience indicates that CAPS can be performed under local or general anesthesia, as permitted or tolerated. In this review of 2,344 patients, 'the overall complication rate was 3.4%. The minor complication rate was 2.6% (6 of 2,344 patients), and the major complication rate was 0.8% (2 of 2,344 patients).' Evidence that underscores how this 'hybrid technique' succesfully combines 'the conservation goals of the AP approach and anatomic virtues of the PA approach to ethmoidectomy.'
PubMed link
Wednesday, April 05, 2006
Blame it all on GERD!
 'Heavner et al., in two animal studies, have demonstrated that exposure of the eustachean tube to simulated gastric content in rodents creates eustachean tube dysfunction. Velepic et al., in two separate studies, have demonstrated a strong correlation of otitis media and GERD. Using a 24-h double pH probe, they found that approximately 60% of the patients had pathologic GERD. In a 2002 study, Tasker et al. demonstrated that middle-ear effusions taken from 54 children contained pepsin/pepsinogen at concentrations up to 1000-fold greater than those in serum 83% of the time. These data suggest that the reflux of gastric juices could be a major cause for otitis media with effusion in children. The link between otitis media with effusion and pharyngeal reflux was further strengthened in a 2004 study by Keles et al. This dual-probe pH study demonstrated that 48% of the children with chronic otitis media effusion had GERD and 64% of the children had pharyngeal reflux. This study suggests that pharyngeal reflux may play an important role in the causes of chronic otitis media with effusion and also that standard single-channel pH probes evaluating for gastroesphageal reflux frequently will miss pharyngeal reflux.'
'Heavner et al., in two animal studies, have demonstrated that exposure of the eustachean tube to simulated gastric content in rodents creates eustachean tube dysfunction. Velepic et al., in two separate studies, have demonstrated a strong correlation of otitis media and GERD. Using a 24-h double pH probe, they found that approximately 60% of the patients had pathologic GERD. In a 2002 study, Tasker et al. demonstrated that middle-ear effusions taken from 54 children contained pepsin/pepsinogen at concentrations up to 1000-fold greater than those in serum 83% of the time. These data suggest that the reflux of gastric juices could be a major cause for otitis media with effusion in children. The link between otitis media with effusion and pharyngeal reflux was further strengthened in a 2004 study by Keles et al. This dual-probe pH study demonstrated that 48% of the children with chronic otitis media effusion had GERD and 64% of the children had pharyngeal reflux. This study suggests that pharyngeal reflux may play an important role in the causes of chronic otitis media with effusion and also that standard single-channel pH probes evaluating for gastroesphageal reflux frequently will miss pharyngeal reflux.' Should we blame everything on GERD? The above discussion, excerpted from 'SPECIAL COMMENTARY: Should otolaryngologists perform pH probe studies?' by Craig W. Senders in Current Opinion in Otolaryngology & Head and Neck Surgery 2006, 14:38–40 seems to say so.
Should we blame everything on GERD? The above discussion, excerpted from 'SPECIAL COMMENTARY: Should otolaryngologists perform pH probe studies?' by Craig W. Senders in Current Opinion in Otolaryngology & Head and Neck Surgery 2006, 14:38–40 seems to say so.In the past decade or so, more and more 'mysterious' diseases of ENT are finding its origin in acid. From globus pharyngicus, recurrent tonsillitis, chronic pharyngitis to sinusitis. Now, good old 'glue ear' has a new culprit to blame. And which otolaryngologist hasn't been wondering along those lines? It seems in the fragmented world of subspecialised medicine, diseases are pulling us back together!
Heavner SB, Hardy SM, White DR, et al. Function of the eustachian tube
after weekly exposure to pepsin/hydrochloric acid. Otolaryngol Head Neck
Surg 2001; 125:123–129.
Velepic M, Rozmanic V, Velepic M, Bonifacic M. Gastroesophageal reflux, allergy
and chronic tubotympanal disorders in children. Int J Pediatr Otorhinolaryngol
2000 Oct 16; 55 (3):187–190
Velepic MM, Velepic MS, Starcevic R, et al. Gastroesophageal reflux and sequelae
of chronic tubotympanal disorders in children. Acta Otolaryngol 2004
Oct; 124 (8):914–917
Tasker A, Dettmar PW, Panetti M, et al. Is gastric reflux a cause of otitis
media with effusion in children? Laryngoscope 2002 Nov; 112 (11):1930–
1934
Keles B, Ozturk K, Gunel E, et al. Pharyngeal reflux in children with chronic
otitis media with effusion. Acta Otolaryngol 2004 Dec; 124 (10):1178–
1181
Tuesday, October 18, 2005
HIgh frequency hearing loss from low frequency noise
PubMed
Effects of gastroesophageal reflux disease in laryngeal carcinoma
An Italian retrospective investigates the association with 36 consecutive non-smoking and non-drinking patients with histologically confirmed SCC of the larynx vs a control, a group of 125 lifetime non-smoking and non-drinking cancer-free subjects. Patients with laryngeal cancer had a higher prevalence of gastroesophageal reflux disease than the control subjects (P < 0.0001).
PubMed
Thursday, October 13, 2005
New centre for deafness research
The Deafness, Cognition and Language Research Centre (DCAL) will be based at University College London and will be funded by a 4.5m grant from the Economic and Social Research Council (ESRC), it was announced yesterday.
The aim of the centre is to create "a world-class hub of excellence" that will connect research into neuroscience and linguistics to issues affecting deaf individuals in their communities. It will also seek to challenge the perceptions of deafness and study sign language and communication techniques. All the centre's researchers will be expected to become fluent in British Sign Language.'
EducationGuardian.co.uk
Sunday, August 07, 2005
Medical management of middle ear disease in children less than 2 years of age with sensorineural hearing loss
Above are the recommendations based on a meta-analytic study by Westerberg BD, et al. in J Otolaryngol. 2005 Aug;34 Suppl 2:S64-9.
Wednesday, August 03, 2005
Wherefrom the infection?
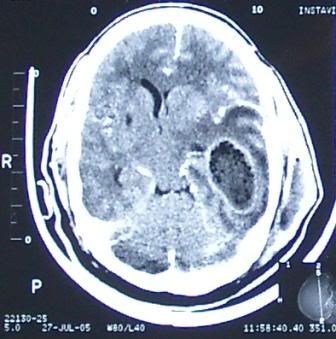 A 55yr-old man had craniectomy and drainage for a huge intracranial temporal lobe abscess and an ipsilateral extracranial temporal abscess as seen in this CT scan. He was referred to ENT for clearance of a possible foci of infection from the mastoid or middle ear which would seem to be the case from the 2nd image presented here. A large area of erosion is seen in the mastoid, communicating with the middle fossa as well as the temporal space.
A 55yr-old man had craniectomy and drainage for a huge intracranial temporal lobe abscess and an ipsilateral extracranial temporal abscess as seen in this CT scan. He was referred to ENT for clearance of a possible foci of infection from the mastoid or middle ear which would seem to be the case from the 2nd image presented here. A large area of erosion is seen in the mastoid, communicating with the middle fossa as well as the temporal space.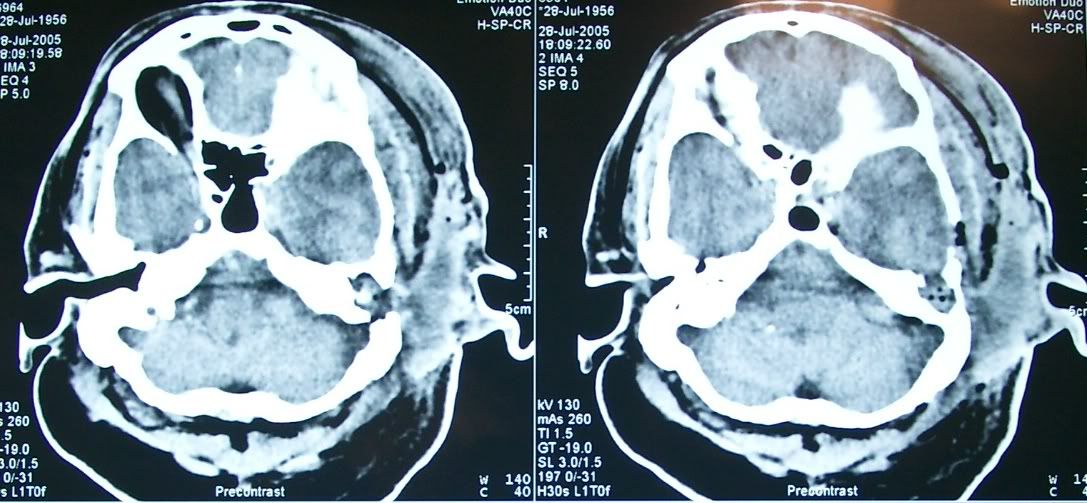
The history, however, was not quite so convincing. He had no history of chronic ear discharge, and was not diabetic. The only lead was one experience of external ear infection 3 months ago after he traumatised his ear canal by overenthusiastic cleaning. Examination would show an external canal filled with pus, a sagging posterosuperior meatal wall, a soft and fluctuant postauricular region and a discharging sinus.


I proceeded to perform a mastoid exploration/cortical mastoidectomy but to my surprise found only a sclerotic mastoid and no foci of disease at all. Drilling was carried all the way down to the bony defect where dura is clearly seen. No pus, granulation, or cholesteatomas found.
So where was the foci of infection? How did an abscess of such magnitude, with such extensive destruction of bone come about? We are hoping a HRCT will give us more clues. Could this be a skull base osteomyelitis secondary to otitis externa?
Thursday, March 17, 2005
Genetic Differences Determine Taste Perception
WebMD Medical News
Scientists looked at a specific taste receptor for a bitter substance known as PTC. Small changes in the genes made big differences in the receptor's ability to recognize the bitter chemical. This helps explain why some people can't taste PTC at all while others find it terribly bitter - and still others find it bitter in varying degrees.
Read the full article
Friday, February 25, 2005
Interview: Genes and Deafness
Listen to the interview by Jennifer Ludden
Gene Therapy for Deafness
American scientists have found that the transplant of a specific gene permits the growth of new hair cells in the inner ear.. The technique, which one day could help millions of people worldwide, was described yesterday by Dr Yehoash Raphael of the Kresge Hearing Research Institute, University of Michigan, in the journal Nature Medicine.
Read the FULL ARTICLE





